A | B | C | D | E | F | G | H | CH | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9
| Alpha | |
 | |
| General details | |
|---|---|
| WHO Designation | Alpha |
| Lineage | B1.1.1.7 |
| First detected | Kent, England |
| Date reported | November 2020 |
| Status | Variant of concern |
| Symptoms | |
| |
| Cases map | |
 Legend: 10,000+ confirmed sequences 5,000–9,999 confirmed sequences 1,000–4,999 confirmed sequences 500–999 confirmed sequences 100–499 confirmed sequences 2–99 confirmed sequences 1 confirmed sequence None or no data available | |
| Major variants | |
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
The Alpha variant (B.1.1.7) was[2][3] a SARS-CoV-2 variant of concern. It was estimated to be 40–80% more transmissible than the wild-type SARS-CoV-2 (with most estimates occupying the middle to higher end of this range). Scientists more widely took note of this variant in early December 2020, when a phylogenetic tree showing viral sequences from Kent, United Kingdom looked unusual.[4]
The variant began to spread quickly by mid-December, around the same time as infections surged. This increase is thought to be at least partly because of one or more mutations in the virus' spike protein. The variant was also notable for having more mutations than normally seen.[5] By January 2021, more than half of all genomic sequencing of SARS-CoV-2 was carried out in the UK.[6] This gave rise to questions as to how many other important variants were circulating around the world undetected.[7][8]
On 2 February 2021, Public Health England reported that they had detected " limited number of B.1.1.7 VOC-202012/01 genomes with E484K mutations",[9] which they dubbed Variant of Concern 202102/02 (VOC-202102/02).[10] One of the mutations (N501Y) was also present in Beta variant and Gamma variant. On 31 May 2021, the World Health Organization announced that the Variant of Concern would be labelled "Alpha" for use in public communications.[11][12]
The Alpha variant disappeared in late 2021 as a result of competition from even more infectious variants. In March 2022, the World Health Organization changed its designation to "previously circulating variant of concern".
Classification
Names
The variant is known by several names. Outside the UK it is sometimes referred to as the UK variant or British variant or English variant,[13] despite the existence of other, less common, variants first identified in UK, such as Eta variant (lineage B.1.525). Within the UK, it is commonly referred to as the Kent variant after Kent, where the variant was found.[14][15][16]
In scientific use, the variant had originally been named the first Variant Under Investigation in December 2020 (VUI – 202012/01) by Public Health England (PHE),[17][a] but was reclassified to a Variant of Concern (Variant of Concern 202012/01, abbreviated VOC-202012/01) by Meera Chand and her colleagues in a report published by PHE on 21 December 2020.[b] In a report written on behalf of COVID-19 Genomics UK (COG-UK) Consortium, Andrew Rambaut and his co-authors, using the Phylogenetic Assignment of Named Global Outbreak Lineages (pangolin) tool, dubbed it lineage B.1.1.7,[19] while Nextstrain dubbed the variant 20I/501Y.V1.[20]
The name VOC-202102/02 refers to the variant with the E484K mutation (see below).[10]
Genetic profile
-
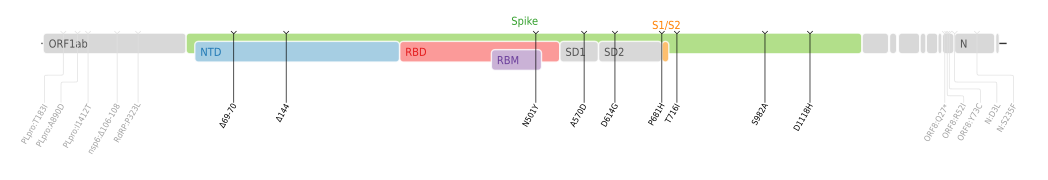
Amino acid mutations of SARS-CoV-2 Alpha variant plotted on a genome map of SARS-CoV-2 with a focus on Spike.[21]
| Gene | Nucleotide | Amino acid |
|---|---|---|
| ORF1ab | C3267T | T1001I |
| C5388A | A1708D | |
| T6954C | I2230T | |
| 11288–11296 deletion | SGF 3675–3677 deletion | |
| Spike | 21765–21770 deletion | HV 69–70 deletion |
| 21991–21993 deletion | Y144 deletion | |
| A23063T | N501Y | |
| C23271A | A570D | |
| C23604A | P681H | |
| C23709T | T716I | |
| T24506G | S982A | |
| G24914C | D1118H | |
| ORF8 | C27972T | Q27stop |
| G28048T | R52I | |
| A28111G | Y73C | |
| N | 28280 GAT→CTA | D3L |
| C28977T | S235F | |
| Source: Chand et al., table 1 (p. 5) | ||
Mutations in SARS-CoV-2 are common: over 4,000 mutations have been detected in its spike protein alone, according to the COVID-19 Genomics UK (COG-UK) Consortium.[22]
VOC-202012/01 is defined by 23 mutations: 14 non-synonymous mutations, 3 deletions, and 6 synonymous mutations[23] (i.e., there are 17 mutations that change proteins and six that do not[5]).
Symptoms and signs
Imperial College London investigated over a million people in England while the Alpha variant was dominant and discovered a wide range of further symptoms linked to Covid. "Chills, loss of appetite, headache and muscle aches" were most common in infected people, as well as classic symptoms.[24]
Diagnosis
Several rapid antigen tests for SARS-CoV-2 are in widespread use globally for COVID-19 diagnostics. They are believed to be useful in stopping the chain of transmission of the virus by providing the means to rapidly identify large numbers of cases as part of a mass-testing program. Following the emergence of VOC-202012/01, there was initially concern that rapid tests might not detect it, but Public Health England determined that rapid tests evaluated and used in the United Kingdom detected the variant.[25]
Prevention
By late 2020, several COVID-19 vaccines were being deployed or under development.
However, as further mutations occurred, concerns were raised as to whether vaccine development would need to be altered. SARS-CoV-2 does not mutate as quickly as, for example, influenza viruses, and the new vaccines that had proved effective by the end of 2020 are types that can be adjusted if necessary.[26] As of the end of 2020, German, British, and American health authorities and experts believe that existing vaccines will be as effective against VOC-202012/01 as against previous variants.[27][28]
On 18 December, NERVTAG determined "that there are currently insufficient data to draw any conclusion on... ntigenic escape".[29]
As of 20 December 2020[update], Public Health England confirmed there is "no evidence" to suggest that the new variant would be resistant to the Pfizer–BioNTech vaccine currently being used in the UK's vaccination programme, and that people should still be protected.[30]
E484K mutation
On 2 February 2021, Public Health England reported that they had detected " limited number of B.1.1.7 VOC-202012/01 genomes with E484K mutations",[9] which is also present in the Beta and Gamma variants;[14] a mutation which may reduce vaccine effectiveness.[14] On 9 February 2021, it became known that some 76 cases with the E484K mutation had been detected, principally in Bristol, but with a genomically distinct group in Liverpool also carrying the mutation.[31] A week later a Research and analysis report from PHE gave a total of 77 confirmed and probable cases involving the E484K mutation across the UK, in two variants, VUI-202102/01 and VOC-202102/02, the latter described as 'B.1.1.7 with E484K'.[10]
On 5 March 2021, it was reported that a B.1.1.7 lineage with the E484K mutation has been detected in two US patients (in Oregon and New York states). Researchers thought that the E484K mutation in the Oregon variant arose independently.[32][33]
Characteristics
Transmissibility
The transmissibility of the Alpha variant (lineage B.1.1.7) had generally been found to be substantially higher than that of pre-existing SARS-CoV-2 variants. The variant was discovered by a team of scientists at COG-UK whose initial results found transmissibility was 70% (50-100%) higher.[16][34] A study by the Centre for the Mathematical Modelling of Infectious Diseases at the London School of Hygiene & Tropical Medicine reported that the variant was 43 to 90% (range of 95% credible intervals, 38 to 130%) more transmissible than pre-existing variants in the United Kingdom, depending on the method used to assess increases in transmissibility. Similar increases in the transmissibility of lineage B.1.1.7 were measured in Denmark, Switzerland, and the United States.[35] Furthermore, a simple model to account for the rapid rise of lineage B.1.1.7 in several countries and the world found that the variant is 50% more transmissible than the local wild type in these three countries and across the world as whole.[36] Another study concluded that it was 75% (70%–80%) more transmissible in the UK between October and November 2020.[37] A later study suggested that these earlier estimates overestimated the transmissibility of the variant and that the transmissibility increase was on the lower ends of these ranges.[38][39]
The Dutch Ministry of Health, Welfare and Sport calculated, based on genome sequencing of positive cases, each week the transmissibility rate of the variant compared to the local wildtype, and found it to fluctuate between 28%-47% higher during the first six weeks of 2021.[40] The Danish Statens Serum Institut in comparison calculated it to be 55% (48%–62%) more transmissible in Denmark based upon the observed development of its relative frequency from 4 January to 12 February 2021.[41] The Institute of Social and Preventive Medicine (ISPM) under University of Bern, calculated the transmissibility of lineage B.1.1.7 based on the weekly development of its observed fraction of all Covid-19 positives during the entire pandemic, and found for 95% confidence intervals under the assumption of a wildtype reproduction number Rw≈1 and an exponentially generation time of 5.2 days, that transmissibility was: 52% (45%–60%) higher when compared to the wildtype in Denmark and 51% (42%-60%) higher when compared to the wildtype in Switzerland.[42]
On 18 December 2020—early on in the risk assessment of the variant—the UK scientific advisory body New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) concluded that they had moderate confidence that VOC-202012/01 was substantially more transmissible than other variants, but that there were insufficient data to reach any conclusion on underlying mechanism of increased transmissibility (e.g. increased viral load, tissue distribution of virus replication, serial interval etc.), the age distribution of cases, or disease severity.[29] Data seen by NERVTAG indicated that the relative reproduction number ("multiplicative advantage") was determined to be 1.74—i.e., the variant is 74% more transmissible—assuming a 6.5-day generational interval. It was demonstrated that the variant grew fast exponentially with respect to the other variants.[43][44][45] The variant out-competed the ancestral variant by a factor of every two weeks. Another group came to similar conclusions, generating a replicative advantage, independent of "protective measures", of 2.24 per generation of 6.73 days, out-competing the ancestral variant by every two weeks.[46] Similarly, in Ireland, the variant—as indicated by the missing S gene[c] detection (S-gene target failure ), which historically was rare—went from 16.3% to 46.3% of cases in two weeks. This demonstrates, based on the statistics of 116 positive samples, that the variant had a relative higher growth by a factor of , when compared to the average growth for all other variants by the end of this two week period.[48] The variant became the dominant variant in London, East of England and the South East from low levels in one to two months. A surge of SARS-CoV-2 infections around the start of the new year is seen[by whom?] as being the result of the elevated transmissibility of the variant, while the other variants were in decline.[49][50][51]
One of the most important changes in lineage B.1.1.7 seems to be N501Y,[22] a change from asparagine (N) to tyrosine (Y) in amino-acid position 501.[52] This is because of its position inside the spike protein's receptor-binding domain (RBD)—more specifically inside the receptor-binding motif (RBM),[53] a part of the RBD[54]—which binds human ACE2.[55] Mutations in the RBD can change antibody recognition and ACE2 binding specificity[55] and lead to the virus becoming more infectious;.[22] Chand et al. concluded that "t is highly likely that N501Y affects the receptor-binding affinity of the spike protein, and it is possible that this mutation alone or in combination with the deletion at 69/70 in the N-terminal domain (NTD) is enhancing the transmissibility of the virus".[56] In early 2021 a peer-reviewed paper found that the mentioned HV 69–70 deletion in vitro "appeared to have two-fold higher infectivity over a single round of infection compared to [wild-type SARS-CoV-2]" in lentiviral SARS-CoV-2 pseudoviruses.[57]
Using In Silico approach, Shahhosseini et al. demonstrated that the Y501 mutation in lineage B.1.1.7 forms a shorter H-bond (length of 2.94 Å) than its counterpart in the wild type (WT) variant residue N501, indicating that in lineage B.1.1.7 the RBD and hACE2 have a stable interaction. Furthermore, the Y501 mutation in lineage B.1.1.7 contributes more negatively to Binding Free Energy (BFE) (-7.18 kcal/mol) than its counterpart in the WT variant residue N501 (-2.92 kcal/mol). As a result of combining BFE and molecular interaction results, the N501Y mutation in RBD strengthens binding affinity of SARS-CoV-2 RBD to hACE2.[58]
In a detailed affinity and kinetic analysis of the interaction between the Spike RBD and ACE2, the N501Y mutation was found to significantly enhance the binding affinity between the RBD and ACE2 by approximately 10-fold, resulting from a 1.8-fold increase in the association rate constant (kon) and a 7-fold decrease in the dissociation rate constant (koff).[59]
Virulence
Matched cohort studies of the Alpha variant (lineage B.1.1.7) found higher mortality rate than earlier circulating variants overall,[60][61] but not in hospitalised patients.[62] An ecological study found no difference in mortality overall.[63]
Initially, NERVTAG said on 18 December 2020 that there were insufficient data to reach a conclusion regarding disease severity. At prime minister Boris Johnson's briefing the following day, officials said that there was "no evidence" as of that date that the variant caused higher mortality or was affected differently by vaccines and treatments;[64] Vivek Murthy agreed with this.[65] Susan Hopkins, the joint medical adviser for the NHS Test and Trace and Public Health England (PHE), declared in mid-December 2020: "There is currently no evidence that this strain causes more severe illness, although it is being detected in a wide geography, especially where there are increased cases being detected."[22] Around a month later, however—on 22 January 2021—Johnson said that "there is some evidence that the new variant ... may be associated with a higher degree of mortality", though Sir Patrick Vallance, the government's Chief Scientific Advisor, stressed that there is not yet enough evidence to be fully certain of this.[66]
In a paper analysing twelve different studies on lineage B.1.1.7 death rate relative to other lineages, it was found to have a higher death rate (71% according to LSHTM, 70% according to University of Exeter, 65% according to Public Health England, and 36% according to Imperial College London), and NERVTAG concluded: "Based on these analyses, it is likely that infection with VOC B.1.1.7 is associated with an increased risk of hospitalisation and death compared to infection with non-VOC viruses".[67] Results of the death studies were associated with some high uncertainty and confidence intervals, because of a limited sample size related to the fact that UK only analysed the VOC status for 8% of all COVID-19 deaths.[68]
A UK case-control study for 54,906 participants, testing positive for SARS-CoV-2 between 1 October 2020 and 29 January 2021 in the community setting (not including vulnerable persons from care centres and other public institutions), reported that patients infected with the Alpha variant (VOC 202012/1) had a hazard ratio for death within 28 days of testing of 1.64 (95% confidence interval 1.32-2.04), as compared with matched patients positive for other variants of SARS-CoV-2.[69] Also in the UK, a survival analysis of 1,146,534 participants testing positive for SARS-CoV-2 between 1 November 2020 and 14 February 2021, including individuals in the community and in care and nursing homes, found a hazard ratio of 1.61 (95% confidence interval 1.42–1.82) for death within 28 days of testing among individuals infected with lineage B.1.1.7; no significant differences in the increased hazard of death associated with lineage B.1.1.7 were found among individuals differing in age, sex, ethnicity, deprivation level, or place of residence.[61] Both studies adjusted for varying COVID-19 mortality by geographical region and over time, correcting for potential biases due to differences in testing rates or differences in the availability of hospital services over time and space.[citation needed]
A Danish study found people infected by lineage B.1.1.7 to be 64% (32%–104%) more likely to get admitted to hospitals compared with people infected by another lineage.[70]
Genetic sequencing of VOC-202012/01 has shown a Q27stop mutation which "truncates the ORF8 protein or renders it inactive".[19] An earlier study of SARS-CoV-2 variants which deleted the ORF8 gene noted that they "have been associated to milder symptoms and better disease outcome".[71] The study also noted that "SARS-CoV-2 ORF8 is an immunoglobulin (Ig)–like protein that modulates pathogenesis", that "SARS-CoV-2 ORF8 mediates major histocompatibility complex I (MHC-I) degradation", and that "SARS-CoV-2 ORF8 suppresses type I interferon (IFN)–mediated antiviral response".[71]
Referring to amino-acid position 501 inside the spike protein, Chand et al. concluded that "it is possible that variants at this position affect the efficacy of neutralisation of virus",[56] but noted that "here is currently no neutralisation data on N501Y available from polyclonal sera from natural infection".[56] The HV 69–70 deletion has, however, been discovered "in viruses that eluded the immune response in some immunocompromised patients",[72] and has also been found "in association with other RBD changes".[56]
Epidemiology


Cases of the Alpha variant (lineage B.1.1.7) were estimated to be under-reported by most countries as the most commonly used tests do not distinguish between this variant and other SARS-CoV-2 variants, and as many SARS-CoV-2 infections are not detected at all. RNA sequencing is required for detection of this variant,[82] although RT-PCR test for specific variants[d] can be used as a proxy test for Alpha — or as a supplementing first-screening test before conducting the whole-genome sequencing.[83][75]
Zdroj:https://en.wikipedia.org?pojem=SARS-CoV-2_Alpha_variant
Text je dostupný za podmienok Creative Commons Attribution/Share-Alike License 3.0 Unported; prípadne za ďalších podmienok. Podrobnejšie informácie nájdete na stránke Podmienky použitia.
Antropológia
Aplikované vedy
Bibliometria
Dejiny vedy
Encyklopédie
Filozofia vedy
Forenzné vedy
Humanitné vedy
Knižničná veda
Kryogenika
Kryptológia
Kulturológia
Literárna veda
Medzidisciplinárne oblasti
Metódy kvantitatívnej analýzy
Metavedy
Metodika
Text je dostupný za podmienok Creative
Commons Attribution/Share-Alike License 3.0 Unported; prípadne za ďalších
podmienok.
Podrobnejšie informácie nájdete na stránke Podmienky
použitia.
www.astronomia.sk | www.biologia.sk | www.botanika.sk | www.dejiny.sk | www.economy.sk | www.elektrotechnika.sk | www.estetika.sk | www.farmakologia.sk | www.filozofia.sk | Fyzika | www.futurologia.sk | www.genetika.sk | www.chemia.sk | www.lingvistika.sk | www.politologia.sk | www.psychologia.sk | www.sexuologia.sk | www.sociologia.sk | www.veda.sk I www.zoologia.sk