A | B | C | D | E | F | G | H | CH | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9
Papillomaviridae is a family of non-enveloped DNA viruses whose members are known as papillomaviruses.[1] Several hundred species of papillomaviruses, traditionally referred to as "types",[2] have been identified infecting all carefully inspected mammals,[2] but also other vertebrates such as birds, snakes, turtles and fish.[3][4][5] Infection by most papillomavirus types, depending on the type, is either asymptomatic (e.g. most Beta-PVs) or causes small benign tumors, known as papillomas or warts (e.g. human papillomavirus 1, HPV6 or HPV11). Papillomas caused by some types, however, such as human papillomaviruses 16 and 18, carry a risk of becoming cancerous.[6]
Papillomaviruses are usually considered as highly host- and tissue-tropic, and are thought to rarely be transmitted between species.[7] Papillomaviruses replicate exclusively in the basal layer of the body surface tissues. All known papillomavirus types infect a particular body surface,[2] typically the skin or mucosal epithelium of the genitals, anus, mouth, or airways.[8] For example, human papillomavirus (HPV) type 1 tends to infect the soles of the feet, and HPV type 2 the palms of the hands, where they may cause warts. Additionally, there are descriptions of the presence of papillomavirus DNA in the blood and in the peripheral blood mononuclear cells.
Papillomaviruses were first identified in the early 20th century, when it was shown that skin warts, or papillomas, could be transmitted between individuals by a filterable infectious agent. In 1935 Francis Peyton Rous, who had previously demonstrated the existence of a cancer-causing sarcoma virus in chickens, went on to show that a papillomavirus could cause skin cancer in infected rabbits. This was the first demonstration that a virus could cause cancer in mammals.
Taxonomy of papillomaviruses

There are over 100 species of papillomavirus recognised,[9] though the ICTV officially recognizes a smaller number, categorized into 53 genera, as of 2019.[10][11][12] All papillomaviruses (PVs) have similar genomic organizations, and any pair of PVs contains at least five homologous genes, although the nucleotide sequence may diverge by more than 50%. Phylogenetic algorithms that permit the comparison of homologies led to phylogenetic trees that have a similar topology, independent of the gene analyzed.[13]
Phylogenetic studies strongly suggest that PVs normally evolve together with their mammalian and bird host species, but adaptive radiations, occasional zoonotic events and recombinations may also impact their diversification.[13] Their basic genomic organization appears maintained for a period exceeding 100 million years, and these sequence comparisons have laid the foundation for a PV taxonomy, which is now officially recognized by the International Committee on Taxonomy of Viruses. All PVs form the family Papillomaviridae, which is distinct from the Polyomaviridae thus eliminating the term Papovaviridae. Major branches of the phylogenetic tree of PVs are considered genera, which are identified by Greek letters. Minor branches are considered species and unite PV types that are genomically distinct without exhibiting known biological differences. This new taxonomic system does not affect the traditional identification and characterization of PV "types" and their independent isolates with minor genomic differences, referred to as "subtypes" and "variants", all of which are taxa below the level of "species".[14] Additionally, phylogenetic groupings at higher taxonomic level have been proposed.[15]
This classification may need revision in the light of the existence of papilloma–polyoma virus recombinants.[16] Additional species have also been described. Sparus aurata papillomavirus 1 has been isolated from fish.[17]
Human papillomaviruses
Over 170 human papillomavirus types have been completely sequenced.[18] They have been divided into 5 genera: Alphapapillomavirus, Betapapillomavirus, Gammapapillomavirus, Mupapillomavirus and Nupapillomavirus. At least 200 additional viruses have been identified that await sequencing and classification.[citation needed]
Animal papillomaviruses

Individual papillomavirus types tend to be highly adapted to replication in a single animal species. In one study, researchers swabbed the forehead skin of a variety of zoo animals and used PCR to amplify any papillomavirus DNA that might be present.[19] Although a wide variety of papillomavirus sequences were identified in the study, the authors found little evidence for inter-species transmission. One zookeeper was found to be transiently positive for a chimpanzee-specific papillomavirus sequence. However, the authors note that the chimpanzee-specific papillomavirus sequence could have been the result of surface contamination of the zookeeper's skin, as opposed to productive infection.[citation needed]
Cottontail rabbit papillomavirus (CRPV) can cause protuberant warts in its native host, the North American rabbit genus Sylvilagus. These horn-like warts may be the original basis for the urban legends of the American antlered rabbit the Jackalope and European Wolpertinger.[20] European domestic rabbits (genus Oryctolagus) can be transiently infected with CRPV in a laboratory setting. However, since European domestic rabbits do not produce infectious progeny virus, they are considered an incidental or "dead-end" host for CRPV.[21]
Inter-species transmission has also been documented for bovine papillomavirus (BPV) type 1.[22] In its natural host (cattle), BPV-1 induces large fibrous skin warts. BPV-1 infection of horses, which are an incidental host for the virus, can lead to the development of benign tumors known as sarcoids. The agricultural significance of BPV-1 spurred a successful effort to develop a vaccine against the virus.[citation needed]
A few reports have identified papillomaviruses in smaller rodents, such as Syrian hamsters, the African multimammate rat and the Eurasian harvest mouse.[23] However, there are no papillomaviruses known to be capable of infecting laboratory mice. The lack of a tractable mouse model for papillomavirus infection has been a major limitation for laboratory investigation of papillomaviruses.[citation needed]
Four papillomaviruses are known to infect birds: Fringilla coelebs papillomavirus 1, Francolinus leucoscepus papillomavirus 1, Psittacus erithacus papillomavirus 1 and Pygoscelis adeliae papillomavirus 1.[24] All these species have a gene (E9) of unknown function, suggesting a common origin.
Evolution
The evolution of papillomaviruses is thought to be slow compared to many other virus types, but there are no experimental measurements currently available. This is probably because the papillomavirus genome is composed of genetically stable double-stranded DNA that is replicated with high fidelity by the host cell's DNA replication machinery.[citation needed]
It is believed that papillomaviruses generally co-evolve with a particular species of host animal over many years, although there are strong evidences against the hypothesis of coevolution.[13][25] In a particularly speedy example, HPV-16 has evolved slightly as human populations have expanded across the globe and now varies in different geographic regions in a way that probably reflects the history of human migration.[26][27] Cutaneotropic HPV types are occasionally exchanged between family members during the entire lifetime, but other donors should also be considered in viral transmission.[28]
Other HPV types, such as HPV-13, vary relatively little in different human populations. In fact, the sequence of HPV-13 closely resembles a papillomavirus of bonobos (also known as pygmy chimpanzees).[29] It is not clear whether this similarity is due to recent transmission between species or because HPV-13 has simply changed very little in the six or so million years since humans and bonobos diverged.[27]
The most recent common ancestor of this group of viruses has been estimated to have existed 424 million years ago.[30]
There are five main genera infecting humans (Alpha, Beta, Gamma, Mu and Nu). The most recent common ancestor of these genera evolved 49.7 million years ago-58.5 million years ago.[31] The most recent ancestor of the gamma genus was estimated to have evolved between 45.3 million years ago and 67.5 million years ago.[citation needed]
Structure
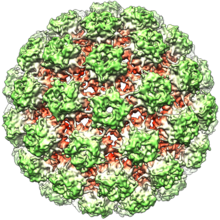
Papillomaviruses are non-enveloped, meaning that the outer shell or capsid of the virus is not covered by a lipid membrane. A single viral protein, known as L1, is necessary and sufficient for formation of a 55–60 nanometer capsid composed of 72 star-shaped capsomers (see figure). Like most non-enveloped viruses, the capsid is geometrically regular and presents icosahedral symmetry. Self-assembled virus-like particles composed of L1 are the basis of a successful group of prophylactic HPV vaccines designed to elicit virus-neutralizing antibodies that protect against initial HPV infection. As such, papillomaviridæ are stable in the environment.[citation needed]
The papillomavirus genome is a double-stranded circular DNA molecule ~8,000 base pairs in length. It is packaged within the L1 shell along with cellular histone proteins, which serve to wrap and condense DNA.[citation needed]
The papillomavirus capsid also contains a viral protein known as L2, which is less abundant. Although not clear how L2 is arranged within the virion, it is known to perform several important functions, including facilitating the packaging of the viral genome into nascent virions as well as the infectious entry of the virus into new host cells. L2 is of interest as a possible target for more broadly protective HPV vaccines.
The viral capsid consists of 72 capsomeres of which 12 are five-coordinated and 60 are six-coordinated capsomeres, arranged on a T = 7d icosahedral surface lattice.[32]
Tissue specificity
Papillomaviruses replicate exclusively in keratinocytes. Keratinocytes form the outermost layers of the skin, as well as some mucosal surfaces, such as the inside of the cheek or the walls of the vagina. These surface tissues, which are known as stratified squamous epithelia, are composed of stacked layers of flattened cells. The cell layers are formed through a process known as cellular differentiation, in which keratinocytes gradually become specialized, eventually forming a hard, crosslinked surface that prevents moisture loss and acts as a barrier against pathogens. Less-differentiated keratinocyte stem cells, replenished on the surface layer, are thought to be the initial target of productive papillomavirus infections. Subsequent steps in the viral life cycle are strictly dependent on the process of keratinocyte differentiation. As a result, papillomaviruses can only replicate in body surface tissues.[citation needed]
Life cycle
Infectious entry
Papillomaviruses gain access to keratinocyte stem cells through small wounds, known as microtraumas, in the skin or mucosal surface. Interactions between L1 and sulfated sugars on the cell surface promote initial attachment of the virus.[33][34] The virus is then able to get inside from the cell surface via interaction with a specific receptor, likely via the alpha-6 beta-4 integrin,[35][36] and transported to membrane-enclosed vesicles called endosomes.[37][38] The capsid protein L2 disrupts the membrane of the endosome through a cationic cell-penetrating peptide, allowing the viral genome to escape and traffic, along with L2, to the cell nucleus.[39][40][41]
Viral persistence and latency
After successful infection of a keratinocyte, the virus expresses E1 and E2 proteins, which are for replicating and maintaining the viral DNA as a circular episome. The viral oncogenes E6 and E7 promote cell growth by inactivating the tumor suppressor proteins p53 and pRb. Keratinocyte stem cells in the epithelial basement layer can maintain papillomavirus genomes for decades.[8]
Production of progeny virus
The current understanding is that viral DNA replication likely occurs in the G2 phase of the cell cycle and rely on recombination-dependent replication supported by DNA damage response mechanisms (activated by the E7 protein) to produce progeny viral genomes.[42] Papillomavirus genomes are sometimes integrated into the host genome, especially noticeable with oncogenic HPVs, but is not a normal part of the virus life cycle and a dead-end that eliminates the potential of viral progeny production.[42]
The expression of the viral late genes, L1 and L2, is exclusively restricted to differentiating keratinocytes in the outermost layers of the skin or mucosal surface. The increased expression of L1 and L2 is typically correlated with a dramatic increase in the number of copies of the viral genome. Since the outer layers of stratified squamous epithelia are subject to relatively limited surveillance by cells of the immune system, it is thought that this restriction of viral late gene expression represents a form of immune evasion.[citation needed]
New infectious progeny viruses are assembled in the cell nucleus. Papillomaviruses have evolved a mechanism for releasing virions into the environment. Other kinds of non-enveloped animal viruses utilize an active lytic process to kill the host cell, allowing release of progeny virus particles. Often this lytic process is associated with inflammation, which might trigger immune attack against the virus. Papillomaviruses exploit desquamation as a stealthy, non-inflammatory release mechanism.[citation needed]
| Genus | Host details | Tissue tropism | Entry details | Release details | Replication site | Assembly site | Transmission |
|---|---|---|---|---|---|---|---|
| Dyoxipapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Omikronpapillomavirus | Porpoises | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyodeltapapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Omegapapillomavirus | Vertebrates | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Nupapillomavirus | Humans | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyomupapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyozetapapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Kappapapillomavirus | Rabbits | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Upsilonpapillomavirus | Vertebrates | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyoetapapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Sigmapapillomavirus | Vertebrates | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Lambdapapillomavirus | Cats; dogs | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Taupapillomavirus | Vertebrates | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Betapapillomavirus | Humans | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Xipapillomavirus | Bovines | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyoepsilonpapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Thetapapillomavirus | Birds | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Etapapillomavirus | Birds | Epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Rhopapillomavirus | Vertebrates | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyothetapapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyoomikronpapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Gammapapillomavirus | Humans | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Alphapapillomavirus | Humans; monkeys | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Sex; contact |
| Zetapapillomavirus | Horses | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Deltapapillomavirus | Ruminants | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyolambdapapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyosigmapapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyorhopapillomavirus | Vertebrates | None | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Psipapillomavirus | Vertebrates | Epithelial: mucous; epithelial: skin | Cell receptor endocytosis | Lysis | Nucleus | Nucleus | Contact |
| Dyokappapapillomavirus | Zdroj:https://en.wikipedia.org?pojem=Papillomaviridae