A | B | C | D | E | F | G | H | CH | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9
| Prenatal testing | |
|---|---|
| Synonyms | Prenatal screening, Prenatal diagnosis, Genetic testing |
| Purpose | To monitor maternal and fetal health and progression, as well as, detect fetal abnormalities during pregnancy. |
Prenatal testing is a tool that can be used to detect some birth defects at various stages prior to birth. Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible.[1] These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts (as in preimplantation genetic diagnosis) or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, trisomy 18, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.
Prenatal screening focuses on finding problems among a large population with affordable and noninvasive methods. Prenatal diagnosis focuses on pursuing additional detailed information once a particular problem has been found, and can sometimes be more invasive. The most common screening procedures are routine ultrasounds, blood tests, and blood pressure measurement. Common diagnosis procedures include amniocentesis and chorionic villus sampling. In some cases, the tests are administered to determine if the fetus will be aborted, though physicians and patients also find it useful to diagnose high-risk pregnancies early so that delivery can be scheduled in a tertiary care hospital where the baby can receive appropriate care.
Prenatal testing in recent years has been moving towards non-invasive methods to determine the fetal risk for genetic disorders. The rapid advancement of modern high-performance molecular technologies along with the discovery of cell-free fetal DNA (cffDNA) in maternal plasma has led to new methods for the determination of fetal chromosomal aneuploidies. This type of testing is referred to as non-invasive prenatal testing (NIPT) or as non-invasive prenatal screening. Invasive procedures remain important, though, especially for their diagnostic value in confirming positive non-invasive findings and detecting genetic disorders.[3] Birth defects have an occurrence between 1 and 6%.[4]
Purpose
There are three purposes of prenatal diagnosis: (1) to enable timely medical or surgical treatment of a condition before or after birth, (2) to give the parents the chance to abort a fetus with the diagnosed condition, and (3) to give parents the chance to prepare psychologically, socially, financially, and medically for a baby with a health problem or disability, or for the likelihood of a stillbirth. Prior information about problems in pregnancy means that healthcare staff as well as parents can better prepare themselves for the delivery of a child with a health problem. For example, Down syndrome is associated with cardiac defects that may need intervention immediately upon birth.[5]
| Name of Test (Category)' | When | Invasivity | How | Turnaround time | Tests/Screens for
~Associated risks | ||
|---|---|---|---|---|---|---|---|
| Routine prenatal tests | Maternal weight | Every checkup appointment | Non-invasive | Scale | Immediately | Baselines, pre-pregnancy weight estimates, tracking weight gain/loss, pattern observation | NA |
| Maternal blood pressure/Preeclampsia screen[6] | Every checkup appointment | Non-Invasive | Blood pressure cuff | Immediately | Pre-eclampsia/hypertension | NA | |
| Maternal urinalysis/urine test screen[7] | Periodically | Non-invasive | Urine collection | ~a few minutes - ~1 week | hCG, diabetes, dehydration, preeclampsia, kidney and bladder infection/disease | NA | |
| Ultrasound[8] | Periodically | Non-invasive/Invasive | Abdominal or Transvaginal | ~1 day - ~1 week | Fetal development, neural tube defects, birth defects, and various other physical abnormalities (see below for specific ultrasound tests) | NA | |
| Fetal heart rate monitoring[9] | Week 12 - onward | Non-invasive | Handheld abdominal doppler or fetoscope | Immediately | Heart rate irregularities | NA | |
| Genetic prenatal rests | Carrier screening (Screen)[10] | Anytime (before or during pregnancy) | Less invasive | Cheek swab or blood draw | ~2–4 weeks | Determining if a parent carries specific genes associated with certain (primarily autosomal recessive) conditions | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. |
| Chorionic villus sampling/Biopsy, CVS (diagnostic)[11] | Week 8 - 14 | Invasive | Transabdominal or transcervical insertion of a needle, forceps or syringe to obtain a fetal placenta tissue sample | ~1–2 weeks | Chromosomal abnormalities, birth defects | Miscarriage, preterm labor/delivery, infection, cramping, bleeding, premature rupture of amniotic membrane, baby limb defects | |
| Cell-free fetal DNA (cfDNA) Test/Noninvasive prenatal test (NIPT) (screen)[12] | Week 10 - onward | Less invasive | Blood draw | ~1–2 weeks | Gender, chromosomal abnormalities | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. | |
| First trimester screening[13] | Week 10 - 13 | Invasive | Nuchal translucency ultrasound & blood prick/draw | ~1 week | Chromosomal abnormalities, birth defects, heart defects | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. | |
| Alpha-fetoprotein (AFP)/modified sequential/multiple marker/quad/triple/maternal serum test (screen)[14] | Weeks 14 - 22 | Less invasive | Blood draw | ~1–2 weeks | Maternal hormone levels, risk of gestational hypertension and preeclampsia, chromosome abnormalities, neural tube defects | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. | |
| Second trimester screening (screen)[15] | Week 15 - 22 | Invasive | Ultrasound and multiple markers or quad screen blood draw | ~1–2 weeks | Chromosomal abnormalities, neural tube defects, abdominal wall defects, heart defects, other major physical defects | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. | |
| Amniocentesis (diagnostic)[16][17] | Week 15 - 20 | Invasive | Transabdominal needle insertion to obtain an amniotic fluid sample | ~2 weeks | Chromosomal abnormalities, autosomal recessive conditions, neural tube defects, abdominal wall defects, birth defects | Miscarriage (1%), preterm labor/delivery, infection, cramping, bleeding, premature rupture of amniotic membrane | |
| Cordocentesis/Percutaneous umbilical cord blood sampling (PUBS) (diagnostic)[18] | Week 17 - onward | Invasive | Fetal blood sample from umbilical cord | ~3 days | Chromosomal abnormalities, blood disorders (fetal hemolytic disease) | Miscarriage (1-2%), preterm labor/delivery, infection, bleeding, decreased fetal heart rate, premature rupture of amniotic membrane, death | |
| Preimplantation genetic diagnosis (PGD) (screen)[19] | During IVF, prior to implantation | Non-invasive | IVF ebryo examination | ~1–2 weeks | Chromosomal abnormalities, autosomal recessive conditions | NA | |
| Additional prenatal tests | Glucose challenge test (screen) | Week 26 - 28 | Less invasive | Maternal blood draw after ingestion of glucose drink | ~1–2 days | To indicate the possibility of gestational diabetes | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. |
| Oral Glucose Tolerance Test (Screen)[20] | Week 26 - 28 | Less invasive | Maternal blood draws before and after injestion of glucose drink, requires fasting | ~2–3 days | To properly diagnose gestational diabetes following an abnormal result from the glucose challenge screen | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. | |
| Non-stress test[21] | Week 28 - onward | Non-invasive | Abdominal contraction/Fetal heart rate belt | Immediately | Fetal heart rate vs movement, oxygen levels (indicating problems stemming from the placenta or umbilical cord), fetal distress | NA | |
| Group B Strep Test[22] | Week 36 - 38 | Invasive | Vaginal swab | ~1–2 days | Bacteria indicating Group B Strep | NA | |
| Cervix dialation check[23] | Week 37 - onward | Invasive | The doctor takes a manual measurement inside the cervix | Immediately | Signs or progress of dialation, prodromal labor | Infection, premature rupture of amniotic membrane | |
| External fetal monitoring[9] | During Labor, after rupture of amnioatic sac | Invasive | Spiral wire electrode attached to body part (typically the scalp) of fetus via cervical insertion | Immediately | Heart rate irregularities, monitoring fetal heart rate | Fetal bruising/infection at attachment site | |
| Kleihauer-Betke/Fetal cells in maternal blood (FCMB) test (screen)[24] | Situational | Less invasive | Blood draw | <1 day | Fetal red blood cells in the mother's blood, fetomaternal hemorrhage | Very low risk, however there is the potential for bruising, pain, nerve damage, fainting, haematoma, bacterial infection, and bloodborne pathogen exposure. |
Prenatal screening
Maternal serum screening
First-trimester maternal serum screening can check levels of free β-hCG, PAPP-A, intact or beta hCG, or h-hCG in the woman's serum, and combine these with the measurement of nuchal translucency (NT). Some institutions also look for the presence of a fetal nasalbone on the ultrasound.
Second-trimester maternal serum screening (AFP screening, triple screen, quad screen, or penta screen) can check levels of alpha fetoprotein, β-hCG, inhibin-A, estriol, and h-hCG (hyperglycosolated hCG) in the woman's serum.
The triple test measures serum levels of AFP, estriol, and beta-hCG, with a 70% sensitivity and 5% false-positive rate. It is complemented in some regions of the United States, as the Quad test (adding inhibin A to the panel, resulting in an 81% sensitivity and 5% false-positive rate for detecting Down syndrome when taken at 15–18 weeks of gestational age).[25]
The biomarkers PAPP-A and β-hCG seem to be altered for pregnancies resulting from ICSI, causing a higher false-positive rate. Correction factors have been developed and should be used when screening for Down's syndrome in singleton pregnancies after ICSI,[26] but in twin pregnancies such correction factors have not been fully elucidated.[26] In vanishing twin pregnancies with a second gestational sac with a dead fetus, first-trimester screening should be based solely on the maternal age and the nuchal translucency scan as biomarkers are altered in these cases.[26]
Advances in prenatal screening
Measurement of fetal proteins in maternal serum is a part of standard prenatal screening for fetal aneuploidy and neural tube defects.[27][28] Computational predictive model shows that extensive and diverse feto-maternal protein trafficking occurs during pregnancy and can be readily detected non-invasively in maternal whole blood.[29] This computational approach circumvented a major limitation, the abundance of maternal proteins interfering with the detection of fetal proteins, to fetal proteomic analysis of maternal blood. Entering fetal gene transcripts previously identified in maternal whole blood into a computational predictive model helped develop a comprehensive proteomic network of the term neonate. It also shows that the fetal proteins detected in pregnant woman's blood originate from a diverse group of tissues and organs from the developing fetus. Development proteomic networks dominate the functional characterization of the predicted proteins, illustrating the potential clinical application of this technology as a way to monitor normal and abnormal fetal development.
The difference in methylation of specific DNA sequences between mother and fetus can be used to identify fetal-specific DNA in the blood circulation of the mother. In a study published in the March 6, 2011, online issue of Nature, using this non-invasive technique a group of investigators from Greece and UK achieved correct diagnosis of 14 trisomy 21 (Down syndrome) and 26 normal cases.[30][31] Using massive parallel sequencing, a study testing for trisomy 21 only, successfully detected 209 of 212 cases (98.6%) with 3 false-positives in 1,471 pregnancies (0.2%).[32] With commercially available non-invasive (blood) testing for Down syndrome having become available to patients in the United States and already available in China, in October 2011, the International Society for Prenatal Diagnosis created some guidance. Based on its sensitivity and specificity, it constitutes an advanced screening test and that positive results require confirmation by an invasive test, and that while effective in the diagnosis of Down syndrome, it cannot assess half the abnormalities detected by invasive testing. The test is not recommended for general use until results from broader studies have been reported, but may be useful in high-risk patients in conjunction with genetic counseling.[33]
A study in 2012 found that the maternal plasma cell-free DNA test was also able to detect trisomy 18 (Edwards syndrome) in 100% of the cases (59/59) at a false-positive rate of 0.28%, and trisomy 13 (Patau syndrome) in 91.7% of the cases (11/12) at a false-positive rate of 0.97%. The test interpreted 99.1% of samples (1,971/1,988); among the 17 samples without an interpretation, three were trisomy 18. The study stated that if z-score cutoffs for trisomy 18 and 13 were raised slightly, the overall false-positive rates for the three aneuploidies could be as low as 0.1% (2/1,688) at an overall detection rate of 98.9% (280/283) for common aneuploidies (this includes all three trisomies: Down, Edwards and Patau).[34]
Prenatal genetic testing
This section has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these template messages)
|
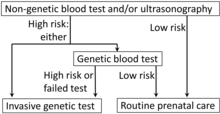
The goal of prenatal genetic testing is to identify pregnancies at high risk of abnormalities, allowing for early intervention, termination or appropriate management and preparation measures.[35] Prenatal genetic testing is done by means of different screens and diagnostic tests. A screen informs an individual of the potential for certain abnormalities occurring, whereas, the diagnostic testing is used to confirm/diagnose specific abnormalities exist within the fetus. Prenatal screens are typically less invasive than prenatal diagnostic tests. They come with much lower risk, however, the results are not as definitive as diagnostic tests. Providers often recommend following up with a diagnostic test upon receipt of a positive result from a specific screen.
Medically invasive techniques are those in which a tool is used to access something inside the body. There are varying degrees of invasiveness, depending on what specimen is required to complete the test. The typical blood draw administered by a healthcare professional is one of the most common invasive medical practices.[36] Since it causes minimal discomfort and there is very low risk associated with the sample collection, a blood draw is considered less invasive. Chorionic villus sampling (CVS) and Amniocentesis are the most invasive prenatal tests because there is greater associated risk and the sample is more difficult to access. These procedures are done via needle insertion into the abdomen in order to collect a sample within the uterus, meaning exceptional care/precision is required.[37] Prenatal genetic testing can identify various chromosomal abnormalities, autosomal conditions, various birth defects, and some fetal blood disorders.
Chromosomal abnormalities result from an abnormal number or structuring of chromosomes. This includes chromosomal deletions, duplications, inversions, and translocations.[38] Some examples of chromosomal abnormalities include:
- Down syndrome (trisomy 21)
- Edwards syndrome (trisomy 18)
- Patau syndrome (trisomy 13)
- Turner syndrome (monosomy X)
- Klinefelter (XXY) syndrome
- Trisomy X (XXX) syndrome
- XYY syndrome
- Pallister–Killian syndrome
- Wolf–Hirschhorn syndrome
- Cri-du-chat syndrome
- WAGR syndrome
- DiGeorge syndrome
- Fragile X syndrome
- Prader-Willi/Angelman syndrome
Autosomal recessive conditions occur when both parents pass on a mutation within an autosomal (non-sex) chromosome.[39] Some examples of autosomal recessive conditions are:
- Cystic fibrosis
- Sickle cell anemia
- Tay–Sachs disease
- Spinal muscular atrophy
- Autosomal recessive polycystic kidney disease
- Phenylketonuria
Neural tube defects are a type of birth defect that occurs when the neural tube of a fetus does not form/close properly, potentially effecting other systems throughout the body.[40] Some examples of neural tube defects are:
Abdominal wall defects are a type of birth defect that occur when the abdominal wall of a fetus does not form properly, potentially effecting other organs throughout the body.[41] Some examples of abdominal wall defects are:
- Gastroschisis
- Omphalocele
- Bladder exstrophy
- Cloacal exstrophy
- Ectopia cordis
- Pentalogy of Cantrell
- Body-stalk anomaly
Blood disorders can occur from a negative interaction between the maternal blood and the fetal blood.[42] An example of a fetal blood disorder is Hemolytic disease of the fetus.
Ultrasound imaging and serum markers as indications for genetic testing
Ultrasound imaging provides the opportunity to conduct a nuchal translucency (NT) scan screening for chromosomal abnormalities such as Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), and Patau syndrome (trisomy 13). Using the information from the NT scan the mother can be offered an invasive diagnostic test for fetal chromosomal abnormalities. Serum markers are utilized in a similar fashion to identify gestations that should be recommended for further testing. When the NT scan or serum markers arouse suspicion for chromosomal abnormalities the following genetic tests may be conducted on fetal or placental tissue samples: Interphase-fluorescence in situ hybridization (FISH), quantitative PCR and direct preparation of chromosomes from chorionic villi.[43]
Screens
Carrier screening
Carrier Screening is a general DNA test that uses a blood or cheek swab sample to determine if the parents carry certain genetic conditions. This test can be done anytime, whether the individual(s) are considering starting a family or have already become pregnant. Various types of carrier screens are available that test for progressively more genetic abnormalities. The single gene/condition screen will test for a specific condition, whereas, the expanded carrier screen will test for hundreds of different abnormalities that can be inherited by a fetus. There are also three gene/condition and ethnic specific carrier tests. In the case of a positive test result, further testing is often recommended, as the carrier test only determines if the parent(s) is a carrier, not if the gene has definitively been passed to the fetus.[10]
Placental acellular DNA (pa-DNA)
Placental acellular (fetal cell-free) DNA testing (pa-DNA) allows for the detection of apoptotic placental cells and placental DNA circulating in maternal blood for the noninvasive diagnosis of fetal aneuploidy.[43][44] A meta-analysis that investigated the success rate of using placental acellular DNA from maternal blood to screen for aneuploidies found that this technique detected trisomy 13 in 99% of the cases, trisomy 18 in 98% of the cases and trisomy 21 in 99% of the cases.[44][45] Failed tests using placental acellular DNA are more likely to occur in fetuses with trisomy 13 and trisomy 18 but not with trisomy 21.[46] Previous studies found elevated levels of acellular placental DNA for trisomy 13 and 21 from maternal serum when compared to women with euploid pregnancies.[47][48][49][50] However, an elevation of acellular DNA for trisomy 18 was not observed.[47] Circulating placental nucleated cells comprise only three to six percent of maternal blood plasma DNA, reducing the detection rate of fetal developmental abnormalities.[50] Two alternative approaches have been developed for the detection of fetal aneuploidy. The first involves the measuring of the allelic ratio of single nucleotide polymorphisms (SNPs) in the mRNA coding region in the placenta. The next approach is analyzing both maternal and placental DNA and looking for differences in the DNA methylation patterns.[12][50]
First/Second/Third trimester Screen
The first, second, combined, and third trimester screens typically consist of an ultrasound (abdominal and/or transvaginal) and maternal blood/serum testing. The ultrasound is used to visually assess the growth, development, and activity of the fetus through imaging observations and measurements. The ultrasound portion of the first trimester screen can include a nuchal translucency screen and a fetal nasal bone determination screen. The available blood tests from the first trimester screen can test for plasma protein A and human chorionic gonadotropin. The second trimester screen looks at specific blood markers, to include the estriol, inhibin and human chorionic gonadotropin hormones and often consists of Alpha-fetoprotein (AFP) screening. Any abnormal results from these screening tests can indicate the possibility of abnormal conditions such as Trisomy 18, Trisomy 21 (Down syndrome), and spina bifida.[13]
Alpha-fetoprotein (AFP)/multiple marker test
The AFP test is often done in the second trimester using the serum from the maternal blood draw. This test looks at a specific protein that is formed in the liver of the fetus and released into the fluid contents of the womb, which is then absorbed into the mother’s blood stream. Multiple determinations stem from the results of AFP testing. Genetically, it can expose chromosomal and neural defects.[51]
Diagnostic tests
Chorionic Villus Sampling (CVS)
CVS is an invasive diagnostic test that can be done during the first trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal abnormalities. A tissue cell sample of the placenta is obtained abdominally via needle or via vaginal insertion of a catheter/syringe into the cervix in combination with ultrasound to guide the procedure. Positive results from CVS require blood testing for confirmation.[51]
Amniocentesis
Amniocentesis is an invasive diagnostic test that can be done during the second trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal and/or neural tube abnormalities. The procedure is typically done via needle, in combination with ultrasound for guidance, to obtain a sample of the amniotic fluid surrounding the fetus.[51]
Cordocentesis/Percutaneous umbilical blood sampling (PUBS)
PUBS is an invasive diagnostic test that can be done during the second trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal and/or blood abnormalities. The demand for cordocentesis tests is diminishing because it has been replaced with CVS and Amniocentesis, which carry less risk. The procedure is typically done via needle into the mother’s abdomen, in combination with ultrasound for guidance, to obtain a blood sample from the umbilical cord of the fetus.[18]
Zdroj:https://en.wikipedia.org?pojem=Prenatal_testing
Text je dostupný za podmienok Creative Commons Attribution/Share-Alike License 3.0 Unported; prípadne za ďalších podmienok. Podrobnejšie informácie nájdete na stránke Podmienky použitia.
Antropológia
Aplikované vedy
Bibliometria
Dejiny vedy
Encyklopédie
Filozofia vedy
Forenzné vedy
Humanitné vedy
Knižničná veda
Kryogenika
Kryptológia
Kulturológia
Literárna veda
Medzidisciplinárne oblasti
Metódy kvantitatívnej analýzy
Metavedy
Metodika
Text je dostupný za podmienok Creative
Commons Attribution/Share-Alike License 3.0 Unported; prípadne za ďalších
podmienok.
Podrobnejšie informácie nájdete na stránke Podmienky
použitia.
www.astronomia.sk | www.biologia.sk | www.botanika.sk | www.dejiny.sk | www.economy.sk | www.elektrotechnika.sk | www.estetika.sk | www.farmakologia.sk | www.filozofia.sk | Fyzika | www.futurologia.sk | www.genetika.sk | www.chemia.sk | www.lingvistika.sk | www.politologia.sk | www.psychologia.sk | www.sexuologia.sk | www.sociologia.sk | www.veda.sk I www.zoologia.sk